Introduction ( How to Control Type 1 Diabetes )
Type 1 diabetes is a chronic condition where the pancreas produces little to no insulin, a hormone essential for regulating blood sugar levels. Unlike Type 2 diabetes, which is often linked to lifestyle factors, Type 1 diabetes is an autoimmune condition that typically develops in childhood or early adulthood. Managing Type 1 diabetes requires a lifelong commitment to monitoring blood sugar levels, maintaining a balanced diet, and using insulin therapy.
Understanding how to control Type 1 diabetes is crucial for preventing complications such as nerve damage, heart disease, and kidney problems. With the right approach, people with Type 1 diabetes can lead healthy, active lives. This article will explore key strategies to effectively manage the condition, including insulin management, dietary choices, exercise, and lifestyle adjustments.
What Is Type 1 Diabetes?
Definition and Causes
Type 1 diabetes is an autoimmune disease in which the body’s immune system mistakenly attacks the insulin-producing beta cells in the pancreas. As a result, the pancreas produces little to no insulin, a hormone that helps regulate blood sugar levels. Without insulin, glucose builds up in the bloodstream instead of being used for energy.
The exact cause of Type 1 diabetes is unknown, but it is believed to be triggered by a combination of genetic and environmental factors. Unlike Type 2 diabetes, which is often linked to obesity and lifestyle choices, Type 1 diabetes is not preventable and can develop at any age, although it is most commonly diagnosed in children and young adults. Some possible triggers include viral infections and immune system abnormalities.
Symptoms and Diagnosis
Recognizing the early signs of Type 1 diabetes is essential for timely diagnosis and treatment. Common symptoms include:
- Frequent urination
- Excessive thirst and dry mouth
- Unexplained weight loss
- Extreme hunger
- Fatigue and weakness
- Blurred vision
- Slow-healing cuts or wounds
- Fruity-smelling breath (a sign of diabetic ketoacidosis)
If these symptoms are present, a doctor will perform various tests to confirm the diagnosis. These may include:
- Fasting Blood Sugar Test: Measures blood glucose levels after fasting overnight.
- Random Blood Sugar Test: Checks blood sugar at any time of the day.
- Glycated Hemoglobin (A1C) Test: Provides an average blood sugar level over the past two to three months.
- Autoantibody Tests: Detects diabetes-related antibodies to differentiate Type 1 from Type 2 diabetes.
Early diagnosis and treatment are crucial in preventing severe complications, such as diabetic ketoacidosis (DKA), a life-threatening condition caused by extremely high blood sugar levels.
How Is Type 1 Diabetes Managed?
Managing Type 1 diabetes requires a combination of insulin therapy, regular blood sugar monitoring, a healthy diet, and lifestyle adjustments. Since the body no longer produces insulin, people with Type 1 diabetes must rely on external insulin and closely monitor their blood glucose levels to maintain stability and prevent complications.
Insulin Therapy: The Cornerstone of Treatment
Insulin therapy is essential for individuals with Type 1 diabetes to regulate blood sugar levels. There are different types of insulin, each working at varying speeds:
- Rapid-acting insulin (e.g., Humalog, NovoLog): Works within minutes and is taken before meals.
- Short-acting insulin (e.g., Regular insulin): Starts working within 30 minutes and lasts a few hours.
- Intermediate-acting insulin (e.g., NPH insulin): Takes longer to start working but lasts up to 12–18 hours.
- Long-acting insulin (e.g., Lantus, Levemir): Provides a steady insulin level throughout the day and night.
- Ultra-long-acting insulin (e.g., Tresiba, Toujeo): Works for over 24 hours for prolonged blood sugar control.
Insulin is typically administered via injections or an insulin pump, which delivers continuous insulin doses throughout the day. The choice of insulin regimen depends on individual needs, lifestyle, and doctor recommendations.
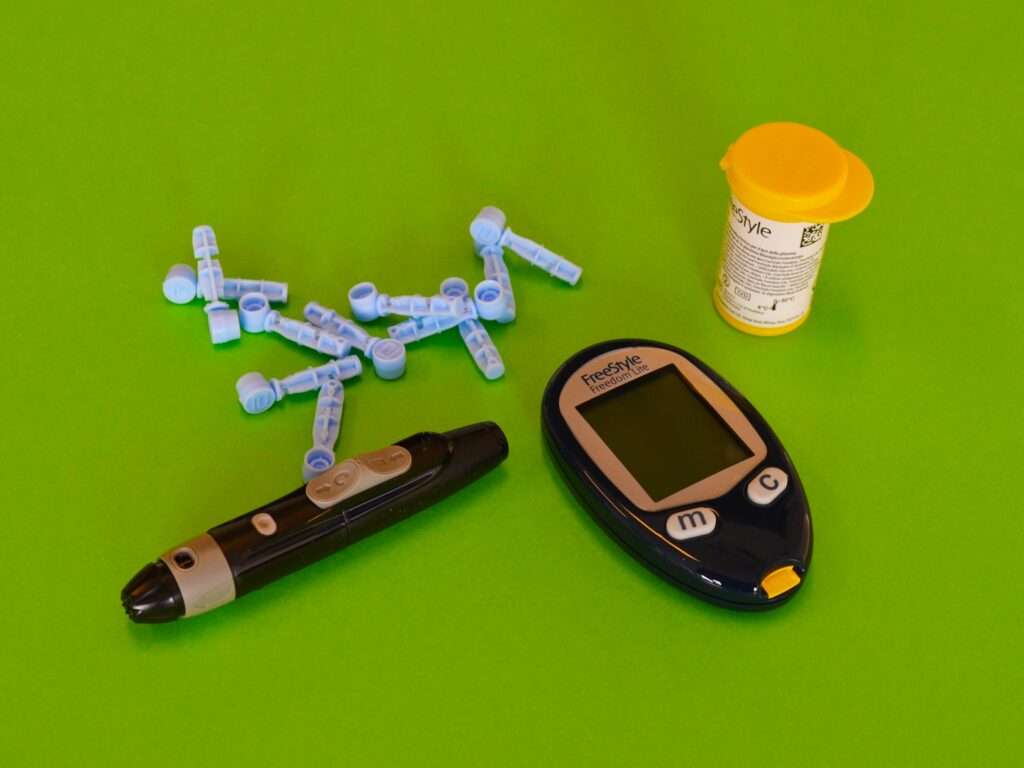
Blood Sugar Monitoring: Tools and Techniques for Regular Checks
Frequent blood sugar monitoring is crucial in managing Type 1 diabetes. Keeping glucose levels within a healthy range helps prevent complications such as nerve damage, kidney disease, and cardiovascular problems. Here are the key methods for tracking blood sugar:
- Fingerstick Testing (Glucometer): A small drop of blood is placed on a test strip inserted into a glucose meter to check blood sugar levels.
- Continuous Glucose Monitors (CGMs): Devices like Dexcom or FreeStyle Libre track blood sugar levels throughout the day without the need for frequent finger pricks.
- Ketone Testing: When blood sugar is very high, ketone testing is necessary to prevent diabetic ketoacidosis (DKA), a severe complication.
Doctors often recommend keeping a blood sugar log to track patterns and make necessary adjustments to insulin doses, diet, and physical activity.
Why Is Blood Sugar Control Crucial?
Maintaining stable blood sugar levels is essential for people with Type 1 diabetes. Proper management not only reduces the risk of serious health complications but also improves overall well-being and quality of life.
Preventing Complications: Long-Term Health Benefits of Stable Blood Glucose Levels
Poorly controlled blood sugar levels can lead to severe health problems over time. Keeping blood glucose within a target range helps prevent:
- Heart Disease and Stroke: High blood sugar levels can damage blood vessels, increasing the risk of heart attacks and strokes.
- Nerve Damage (Neuropathy): Uncontrolled diabetes can lead to nerve damage, causing pain, tingling, or numbness, especially in the hands and feet.
- Kidney Disease (Nephropathy): Excess glucose can harm the kidneys, potentially leading to kidney failure and the need for dialysis.
- Eye Problems (Retinopathy): High blood sugar can damage blood vessels in the eyes, leading to vision loss or blindness.
- Diabetic Ketoacidosis (DKA): A life-threatening condition that occurs when the body breaks down fat too quickly due to a lack of insulin, leading to dangerously high ketone levels in the blood.
By managing blood sugar effectively, individuals with Type 1 diabetes can significantly reduce the risk of these complications and maintain long-term health.
Enhancing Quality of Life: The Positive Impact of Effective Management
When blood sugar is well-controlled, people with Type 1 diabetes experience:
- More Energy: Stable glucose levels prevent the fatigue and weakness associated with high or low blood sugar.
- Better Mood and Mental Clarity: Blood sugar fluctuations can affect brain function and mood, leading to irritability and difficulty concentrating. Proper management supports emotional well-being.
- Improved Physical Health: Maintaining stable blood sugar reduces the risk of infections, enhances wound healing, and supports overall immune function.
- Freedom in Daily Life: With proper diabetes management, individuals can enjoy travel, exercise, and social activities without constant disruptions from blood sugar swings.
By prioritizing blood sugar control, people with Type 1 diabetes can lead active, fulfilling lives while reducing the risk of long-term complications.
How to Control Blood Sugar Levels Effectively
Managing Type 1 diabetes requires a combination of healthy eating, regular exercise, and stress management. By adopting the right strategies, individuals can keep blood sugar levels stable and prevent extreme fluctuations.
Dietary Choices: Foods That Help Maintain Balance
Eating the right foods plays a key role in managing blood sugar levels. A well-balanced diet for Type 1 diabetes should include:
- High-Fiber Foods: Whole grains, beans, vegetables, and fruits help slow glucose absorption and prevent spikes.
- Lean Proteins: Chicken, fish, tofu, eggs, and nuts help maintain energy levels without raising blood sugar.
- Healthy Fats: Avocados, nuts, seeds, and olive oil support heart health and stabilize blood sugar.
- Low-Glycemic Index (GI) Foods: Whole grains, legumes, and non-starchy vegetables provide sustained energy without sudden sugar spikes.
- Hydration: Drinking plenty of water helps the kidneys flush out excess sugar and keeps the body hydrated.
Foods to Avoid:
- Sugary beverages like soda and fruit juices
- Processed snacks and refined carbohydrates (white bread, pasta, pastries)
- Fried and high-fat fast foods
- Excessive alcohol, which can disrupt blood sugar regulation
Physical Activity: Exercise Routines That Aid in Regulation
Regular exercise improves insulin sensitivity and helps maintain stable blood sugar levels. However, it’s important to balance activity with insulin intake to avoid hypoglycemia. Recommended exercises include:
- Aerobic Exercise (Cardio): Walking, jogging, cycling, and swimming help lower blood sugar levels over time. Aim for at least 150 minutes per week of moderate-intensity exercise.
- Strength Training: Lifting weights, using resistance bands, or bodyweight exercises like squats and push-ups improve muscle mass and insulin use.
- Flexibility and Balance Workouts: Yoga and stretching exercises help with stress reduction and overall physical well-being.
Tips for Exercising Safely:
- Check blood sugar levels before and after workouts.
- Carry a quick source of glucose (like fruit or glucose tablets) in case of low blood sugar.
- Stay hydrated and wear proper footwear to prevent injuries.
- Adjust insulin doses if needed, as recommended by a healthcare provider.
Stress Management: Techniques to Keep Stress-Induced Glucose Spikes at Bay
Stress triggers the release of hormones like cortisol and adrenaline, which can raise blood sugar levels. Managing stress effectively can help maintain glucose stability. Here are some techniques to reduce stress:
- Mindfulness and Meditation: Practicing deep breathing, yoga, or guided meditation helps reduce stress hormones.
- Regular Sleep Schedule: Aim for 7–9 hours of quality sleep per night to support overall health and blood sugar regulation.
- Time Management: Planning ahead and setting realistic goals can reduce daily stress.
- Physical Relaxation Techniques: Activities like progressive muscle relaxation, aromatherapy, or listening to calming music can help lower stress levels.
- Social Support: Talking to friends, family, or joining a diabetes support group can provide emotional relief and motivation.
By combining a nutritious diet, regular exercise, and effective stress management techniques, individuals with Type 1 diabetes can maintain stable blood sugar levels and improve their overall quality of life.
What You Need to Do Daily
Managing Type 1 diabetes effectively requires a daily routine to maintain blood sugar stability and prevent complications. By staying consistent with insulin use, monitoring glucose levels, and recognizing warning signs, individuals can lead a healthy and active life.
Establishing a Routine: Consistency in Insulin Administration and Monitoring
A structured daily routine helps prevent unexpected blood sugar fluctuations. Key habits to include:
- Insulin Administration: Follow a consistent schedule for insulin injections or pump usage as prescribed by your doctor. This prevents sudden blood sugar spikes or drops.
- Regular Blood Sugar Monitoring: Use a glucometer or continuous glucose monitor (CGM) to check blood sugar levels multiple times a day, especially before meals, after exercise, and before bedtime.
- Balanced Meal Planning: Eating at the same times each day and maintaining a carbohydrate-consistent diet helps stabilize glucose levels.
- Hydration and Physical Activity: Drink enough water and engage in regular exercise to support insulin sensitivity and overall health.
- Tracking and Adjustments: Keep a diabetes journal or use mobile apps to record insulin doses, meals, exercise, and glucose readings. This helps in identifying patterns and making necessary adjustments.
Recognizing and Responding to Symptoms: Knowing When to Seek Medical Attention
Understanding the symptoms of high and low blood sugar levels is essential for taking quick action.
Signs of High Blood Sugar (Hyperglycemia):
- Increased thirst and frequent urination
- Blurry vision
- Fatigue and weakness
- Headaches
- Fruity-smelling breath (a sign of diabetic ketoacidosis, a medical emergency)
What to Do:
- Check blood sugar levels immediately.
- Take a correction dose of insulin if advised by your doctor.
- Drink water to help flush excess glucose from the bloodstream.
- Seek emergency care if symptoms worsen or ketones are detected in urine.
Signs of Low Blood Sugar (Hypoglycemia):
- Dizziness or shakiness
- Sweating
- Hunger
- Confusion or difficulty concentrating
- Rapid heartbeat
What to Do:
- Consume 15 grams of fast-acting carbohydrates (such as glucose tablets, fruit juice, or candy).
- Recheck blood sugar after 15 minutes. If still low, repeat treatment.
- If unconscious or unable to swallow, someone should administer glucagon and seek medical help immediately.
By staying consistent with insulin management, monitoring blood sugar, and recognizing symptoms, individuals with Type 1 diabetes can prevent complications and maintain good health.
Advanced Management Strategies
For individuals with Type 1 diabetes, advanced management tools like Continuous Glucose Monitors (CGMs) and insulin pumps can enhance blood sugar control, reduce complications, and improve overall quality of life. These technologies help minimize fluctuations and provide a more precise, automated approach to diabetes management.
Continuous Glucose Monitors (CGMs): Benefits and Usage
A Continuous Glucose Monitor (CGM) is a wearable device that tracks blood sugar levels in real-time, providing constant feedback without the need for frequent finger-prick tests.
Benefits of Using a CGM:
- Real-Time Blood Sugar Monitoring: Displays glucose levels every few minutes, helping users make immediate adjustments.
- Hypoglycemia and Hyperglycemia Alerts: Sends alerts when blood sugar levels are too high or too low, reducing the risk of dangerous fluctuations.
- Trend Analysis: Tracks patterns over time, helping individuals and doctors adjust insulin doses and meal plans accordingly.
- Reduced Need for Fingersticks: While occasional calibration may be required, CGMs significantly decrease the need for manual blood sugar checks.
How to Use a CGM:
- A tiny sensor is inserted under the skin (usually on the arm or abdomen) and measures glucose levels from interstitial fluid.
- The sensor transmits data to a receiver or smartphone app, displaying blood sugar trends.
- Some CGMs integrate with insulin pumps, creating an automated insulin delivery system.
Insulin Pumps: How They Work and Their Advantages
An insulin pump is a small, computerized device that delivers continuous, customized insulin doses throughout the day, mimicking the pancreas’s natural function.
How Insulin Pumps Work:
- A thin tube (catheter) is inserted under the skin and connected to a small pump worn on the body.
- The pump delivers basal insulin continuously and bolus insulin before meals or to correct high blood sugar levels.
- Some modern pumps connect with CGMs, automatically adjusting insulin delivery based on real-time glucose readings (hybrid closed-loop system).
Advantages of Insulin Pumps:
- Better Blood Sugar Control: Delivers insulin in precise amounts, reducing spikes and crashes.
- More Flexibility in Lifestyle: No need for multiple daily injections—users can adjust doses easily based on meals and activity levels.
- Reduced Risk of Hypoglycemia: Advanced pumps can predict and prevent low blood sugar episodes.
- Convenience and Comfort: Some pumps are tubeless (patch-style) and can be controlled remotely via smartphone apps.
Choosing the Right Advanced Technology
Both CGMs and insulin pumps can improve diabetes management, but choosing the right option depends on personal preference, lifestyle, and medical advice. Many people use both devices together for a more automated and efficient approach to managing Type 1 diabetes.
Lifestyle Modifications for Better Control
Effectively managing Type 1 diabetes goes beyond medication—it involves lifestyle changes that help maintain stable blood sugar levels while allowing for a fulfilling life.
Integrating Diabetes Management into Daily Life
Balancing diabetes management with work, social activities, and personal commitments can be challenging, but with the right strategies, it becomes manageable.
- Work and School Adjustments: Informing employers, teachers, or colleagues about diabetes can help create a supportive environment. Keeping snacks and a glucose monitor on hand is crucial.
- Social Gatherings and Dining Out: Research restaurant menus in advance, choose balanced meals, and monitor carbohydrate intake to prevent unexpected blood sugar spikes.
- Exercise and Physical Activities: Regular movement is essential but should be paired with careful blood sugar monitoring. Carry fast-acting carbohydrates to prevent hypoglycemia.
- Sleep and Stress Management: Lack of sleep and stress can impact glucose levels. Establishing a bedtime routine and practicing mindfulness or meditation can help maintain stability.
Traveling with Diabetes: Planning and Precautions
Traveling with diabetes requires extra preparation to ensure a smooth experience.
- Packing Essentials: Carry extra insulin, test strips, CGM sensors, and glucose tablets in case of delays.
- Airport Security: Inform TSA agents about medical devices like insulin pumps and CGMs.
- Time Zone Adjustments: When traveling across time zones, consult a healthcare professional to adjust insulin schedules accordingly.
- Emergency Planning: Identify nearby pharmacies and hospitals at your destination in case of emergencies.
Support Systems and Resources
A strong support system is essential for managing Type 1 diabetes effectively.
Connecting with Healthcare Professionals
Building a reliable care team ensures access to expert guidance and personalized treatment plans.
- Endocrinologists: Specialists who help fine-tune insulin therapy and monitor long-term health.
- Diabetes Educators: Professionals who teach essential skills for managing diabetes effectively.
- Dietitians/Nutritionists: Experts who guide meal planning and carbohydrate management.
- Mental Health Professionals: Managing diabetes can be emotionally challenging; therapists or counselors can provide coping strategies.
Joining Support Groups
Connecting with others who have Type 1 diabetes can provide motivation, encouragement, and valuable tips.
- Online Communities: Platforms like Facebook groups, Reddit forums, and diabetes-focused apps allow for virtual support.
- Local Diabetes Support Groups: In-person meetups help individuals share experiences and learn from one another.
- Advocacy and Awareness Organizations: Groups like the American Diabetes Association (ADA) and JDRF (Juvenile Diabetes Research Foundation) offer resources, research updates, and community events.
Conclusion
Embracing a Positive Outlook: Living Well with Type 1 Diabetes
While managing Type 1 diabetes requires daily attention, it doesn’t have to limit one’s quality of life. With the right tools, habits, and support system, individuals can lead fulfilling, active lives.
Continuous Learning and Adaptation
Medical advancements in diabetes management, including artificial pancreas systems and new insulin delivery methods, continue to improve. Staying informed about the latest research and treatments ensures better long-term health.
Final Thought: Type 1 diabetes is a journey, not a limitation. With proactive care and a positive mindset, individuals can live life to the fullest while keeping their blood sugar levels under control.






